

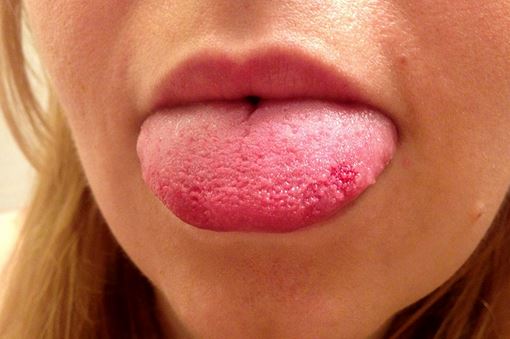
Although they are modified epithelial cells and not quite neurons in vertebrates, taste receptor cells are similar to neurons ( 6). A single cell may be innervated by multiple afferent nerve fibers, and a single fiber may synapse with a multitude of cells. Afferent nerve fibers from cranial nerves VII, IX, and X penetrate the basal surface of the taste bud to innervate the taste receptor cell. Apical microvilli allow gustatory stimuli to interact with the taste receptor cells. The taste bud is concentrically arranged around a pore that opens through the epithelium into the oropharynx. Typically, taste receptor cells are replaced approximately every 2 weeks ( 7). The basal cell, which forms the base of the taste bud and can proliferate to replace taste receptor cells.
Finally, we analyze the available clinical evidence to make recommendations to anesthesia practitioners. The purpose of this review, based on the available peer-reviewed literature, is to summarize the physiology of taste, smell, gustation and olfaction, and to perform a literature review for prior reports of postoperative alterations in taste and smell. Patients with anosmia and ageusia have been known to increase long-term intake of sugar and salt, resulting in worsening of chronic medical conditions such as diabetes mellitus, renal disease, and hypertensive disorders ( 5).

Regardless of cause, these symptoms, albeit usually lasting only 1-2 weeks, can greatly impact one’s quality of life.

In this regard, the incidence of anosmia or ageusia after an anesthetic has been estimated to be approximately 1.8% ( 4). However, anesthetic drugs have also been implicated in cases of anosmia and/or ageusia. The overall incidence of this rare complication has been estimated to be 0.05% and is frequently associated with cardiovascular medications ( 3). Anosmia, the loss of smell, and ageusia, the loss of taste, are rare side effects that can occur as a result of administration of practically all classes of medications ( 1, 2).


 0 kommentar(er)
0 kommentar(er)
